Download PDF
Is an escalating epidemic moving myopia from an optical inconvenience to a crisis calling for preventive measures? Myopia researchers certainly think so.
Until recently, it appeared that the myopia epidemic was flying below ophthalmology’s radar—at least in certain areas of the world. However, with a global prevalence twice that of obesity, no medical condition can quite compare, said Ian Flitcroft, DPhil, FRCOphth, at the Children’s University Hospital in Dublin, Ireland. Although the prevalence of myopia is relatively low in countries such as Australia, he said, it is approaching 40% in the United States and an alarming 80% to 90% in urban areas of East and Southeast Asia.
Optical inconvenience? “It’s amazing that we’ve accepted such huge numbers of people having a condition that requires correction in order for them to perform normally,” he said. “We’re so good at correcting myopia with glasses, contacts, or laser surgery, we’ve come to think of it as simply an optical inconvenience.”
In many countries, however, nothing could be further from the truth, said Nathan G. Congdon, MD, MPH, at Sun Yat-sen University in Guangzhou, China. “In China, only 20% of children who need glasses actually have them, in part, because parents and authorities worry that glasses will harm children’s vision. Providing spectacles for kids not only helps their vision, but we’ve also found that it has a significant impact on their educational outcomes,” he said.1
The long view. Although important, correction of refractive error does nothing to slow the axial growth of the eyeball and related complications of myopia, which are among the top 5 causes of vision loss for working age populations in several countries, said Dr. Flitcroft.
“We re looking at the tip of the iceberg,” agreed Donald Tan, MD, FRCS, FRCOphth, at the Singapore National Eye Center. “We know that complications of pathologic high myopia include macular degeneration, glaucoma, cataract, retinal degeneration—all potentially blinding.” A high myope will have 10 times the risk of a retinal detachment as someone without myopia, added Dr. Flitcroft.
Even within the range of nearsightedness that’s considered physiologic (less than –6 D) rather than pathologic, myopia is one of the biggest risk factors for major eye diseases, said Dr. Flitcroft. “In fact, myopia has as significant an effect on ocular health as hypertension does on cardiovascular health.”
Despite these data, ophthalmologists until recently didn’t even include refractive error when reporting in population studies on the prevalence of the leading causes of blindness, said Prof. Congdon.
It’s past time to bring myopia into the mainstream, suggest 6 myopia researchers, especially now that new approaches are becoming available to slow its progression.
 |
|
Eyeglasses and Education. In China, only 1 in 5 children who need glasses have them. But research here shows that correcting vision significantly affects educational outcomes, said Dr. Congdon.
|
Emmetropia and Myopia
Through a process called emmetropization, the eye is programmed to grow just long enough for light entering the eye to be brought into focus on the retina (or slightly behind it, promoting mild hyperopia), said Prof. Congdon. Across a range of species—from chickens to monkeys to humans—the retina detects and uses hyperopic and myopic defocus to control axial eye growth, added Dr. Flitcroft.
A peripheral issue? Supported by clinical research, animal studies have shown that emmetropization is influenced by retinal images across a wide area, not just the fovea.2 “The peripheral retina seems to guide emmetropization more than the macula,” said Terri L. Young, MD, MBA, a pediatric ophthalmologist and geneticist at the University of Wisconsin in Madison. “This discovery has driven the development of new types of spectacles and contact lenses to slow myopia by addressing the refractive disparity between the macula and periphery.”
Gone awry. Although uncommon, refractive errors present at age 6 are primary failures of emmetropization. Most myopia develops later, which means it is commonly due to a secondary failure of the mechanisms to maintain emmetropia.3
At a certain point—and continuing for a decade or more from childhood to early adulthood—something triggers these eyes into an accelerated growth pattern, said Dr. Flitcroft. “Either something in our current lifestyle prevents the process from working normally, or what we do with our eyes sends confused signals into this control mechanism, driving our eyes to become myopic. In other words, either the ‘thermostat’ is broken or the ‘set point’ is wrong.”
An interruption of this feedback mechanism can also occur when a baby has a condition that blurs image clarity, said Dr. Young. This could be from a vitreous hemorrhage, cataract, or corneal opacification, for example. “The involved eye often grows longer—registered as a myopic shift—than the uninvolved eye.”
 |
|
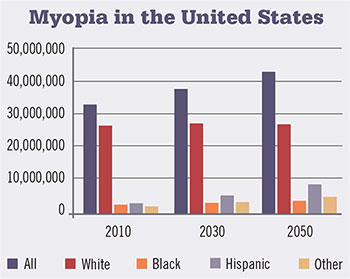
The NEI’s projections for myopia in the United States.
|
Environmental Links to Myopia
What is interfering with the natural course of emmetropization and fueling the myopia epidemic? Researchers have looked at many potential environmental factors. The following theories have more supportive evidence than others, although causation is elusive and many unanswered questions remain.
Time outdoors. “About 20 papers have confirmed that kids who get outside more are less likely to be myopic,” said scientist Ian G. Morgan, PhD, at the Australian National University in Canberra. A recent meta-analysis showed that children with normal vision or hyperopia spent on average 3.7 more hours per week outdoors than those with myopia.4
Theories. Three theories have been offered to explain the visual value of the great outdoors, said Prof. Morgan. One group has argued that light toward the UV end of the spectrum slows eye growth and myopia. A dioptric space theory comes from scientists such as Dr. Flitcroft, who point to the significant differences in defocus across the visual field that are associated with viewing distances in indoor and outdoor environments.5 And through the Sydney Myopia Study Group, Prof. Morgan and colleague Kathryn A. Rose, PhD, offer the light-dopamine theory: Bright outdoor light stimulates the release of dopamine from the retina. In turn, the dopamine signals the sclera to inhibit axial growth.
Light-dopamine. The last of these theories has attracted experimental support. In the laboratory, investigators have created experimental myopia in chickens and nonhuman primates; development of this myopia can be completely inhibited simply by increasing the intensity of light, said Prof. Morgan. “In another experiment using an animal model of myopia, blocking the effects of dopamine with a dopamine antagonist also blocked its protective effect.”
In these studies, he emphasized, the viewing distances of the animals didn’t vary. In addition, essentially UV-free lights were used, reducing the plausibility of the UV theory.
Progression and light exposure. “We don’t yet know whether light also prevents progression of myopia,” said Prof. Morgan. “However, research conducted in Boston—where there’s a big diurnal variation—shows that progression is 3 to 4 times faster in winter than in summer.”
Although it’s not entirely clear how light helps, said Dr. Young, secondary measurements of light exposure do help support epidemiologic studies pointing to light. A 2014 study she coauthored found an inverse relationship between myopic refractive error and ocular sun exposure. There was more than double the prevalence of myopia in the lowest quartile of conjunctival UV autofluorescence—which is linked with amount of sun exposure—than in the highest quartile (33.0% vs. 15.6%), and differences remained significant after adjusting for potential confounders.6
The Outdoor Edge
Go outside and play! In both Singapore and Taiwan, schools are taking outdoor time more seriously, said Prof. Morgan. Although extra outside time is voluntary in Singapore, he said, in Taiwan, the school curriculum requires a minimum of 2 hours outside.
It is likely not a coincidence, he said, that Chinese Australian kids in Sydney, where myopia prevalence is less than 10% at the end of primary school, play outside 3 to 4.5 hours a day, while kids in Singapore report being outside as little as a half hour daily. “By the time they finish primary school in Singapore,” said Prof. Morgan, “50% to 60% are myopic.”
 Bring light inside. Getting kids outside, though, is easier said than done, said Prof. Morgan, especially in cultures where educational success is the top priority or recess is down played lunchtime is sleep time in China, for example. That’s why researchers such as Profs. Morgan and Congdon are searching for ways to bring more natural light indoors. Bring light inside. Getting kids outside, though, is easier said than done, said Prof. Morgan, especially in cultures where educational success is the top priority or recess is down played lunchtime is sleep time in China, for example. That’s why researchers such as Profs. Morgan and Congdon are searching for ways to bring more natural light indoors.
“Extrapolation from experimental work around light suggests kids need about 10,000 lux illumination to slow myopia,” said Prof. Morgan, “but that’s a far cry from the 800 lux of even a well lit classroom.”
He and Prof. Congdon just collaborated on a pilot project in which they put several hundred kids in glass classrooms. “We wanted to first explore its feasibility from a standpoint of temperature, comfort, and reading,” said Prof. Congdon. “We’re next hoping to conduct a randomized trial.”
Although largely popular with students and teachers, the glass classroom provided about 15,000 lux, said Prof. Morgan, which can create a heat problem one that is manageable, according to Prof. Congdon. “One alternative we will also test over the next few years,” said Prof. Morgan, “is a specially engineered lamp that can create 10,000 lux, limited to the desk surface.”
|
An ongoing debate. “We can’t rule out the possibility that a combination of factors is responsible [for outdoor benefits],” said Prof. Morgan. “However, UV light has no effect on emmetropization, which suggests this theory can be ruled out. And there’s no evidence to suggest that accommodation or dioptric space is a secondary mechanism.”
Dr. Flitcroft is unconvinced, however, that light is the exclusive star in this outdoor scenario. Making light the only factor “ignores 30 years of research,” he said, “which shows that a complex vision-dependent process controls axial eye growth. We need to ask ourselves whether being outdoors is an advantage simply because there’s more light or because being outdoors also changes what happens to the peripheral retina.”
One major challenge for the light hypothesis, he said, is that high light levels changed the amount of myopia in only 1 animal model of myopia—deprivation myopia induced by covering an eye with a translucent occluder. High light levels did not change the amount of myopia induced in animals reared with lenses.
 |
Time Outdoors. Children with normal vision or hyperopia spend 3.7 hours per week more than those with myopia, according to a meta-analysis.
|
Near work. “The corollary to time outdoors is that time indoors involves near work,” said Prof. Tan. “We were able to show that children who spent a lot of time with near work—whether reading, writing, or playing computer games—also were at higher risk of developing myopia.”
Near work was the prevailing theory for some time—especially in urban Asia, said Dr. Young—and was thought to be linked to intense educational instruction for long periods. The link between myopia and education is very strong, agreed Prof. Morgan. “The children most at risk are those who combine a lot of near work with little time outdoors.”
Although the popularity of electronic media used inside at close distances may make it harder to slow or reverse the increasing prevalence of myopia, he said, it’s clear that the epidemic predates the widespread adoption of computers, smart phones, tablets, and handheld video games. “By the 1990s, young adults in East and Southeast Asia were already highly myopic.”
Where Genes Come Into Play
There are certainly individuals with a genetic propensity for myopia, said Prof. Congdon.
A combination of influences. “But genetic changes happen slowly, so they can’t explain the rapid rises we’re experiencing.” Where prevalence is particularly high, such as in Hong Kong or Taiwan, most would agree that a combination of genetics and environmental factors are contributing, he said.
With regard to the genetics part of the equation, said Dr. Flitcroft, a big breakthrough came when many genes linked to myopia were identified with studies conducted by the Consortium for Refractive Error and Myopia (CREAM) and 23andMe, a saliva-based DNA service. “In families with high myopia, there are likely changes in the scleral wall connective tissue or in retinal signaling,” said Dr. Young. “Multiple gene mutations have been reported more commonly in those 2 functional areas.” However, said Prof. Morgan, the prevalence of high myopia has increased dramatically in East Asia, which means environmentally induced myopes can also progress to high myopia.
The relevance of genetics. Genetics may become more relevant if we can use markers to identify the kids on the edge of near sightedness who will likely end up with, say, –10 D of myopia, said Dr. Flitcroft. “With these kids, we should do everything in our power to slow their progression get them outdoors, prescribe contact lenses, apply atropine. If we did this, we might keep them at –4 D, and that would be a great result.”
|
Education. Education is also one of the stronger risk factors for myopia, said Katie M. Williams, MPhil, FRCOphth, a researcher at King’s College London, who was lead author on a recent paper analyzing myopia prevalence in Europe. Conducted through the European Eye Epidemiology (E3) Consortium—a group of 30 studies that share and meta-analyze eye phenotypes—the retrospective study examined data from more than 60,000 people with refractive error.7
It found a significant increase in myopia over the latter part of the last century. Although not fully explanatory, education was also strongly associated with myopia prevalence. “Those going on for a university education were twice as likely to be myopic as those who received [only] a primary school education,” said Dr. Williams, “but the increase in myopia prevalence was seen across all levels of education and all birth decades.”
Education is a complicated, multifaceted factor, she cautioned, and this makes it difficult to tease apart what’s actually responsible for the connection to myopia. “Those going on to higher education probably spend more time indoors and more time on near work, computers, and reading,” she said. “They might also be more intelligent than someone who left school earlier. We have also seen changes in educational practices in the last hundred years, where kids have a longer school day, slightly shorter break times, and extra classes, and often start school at younger ages.”
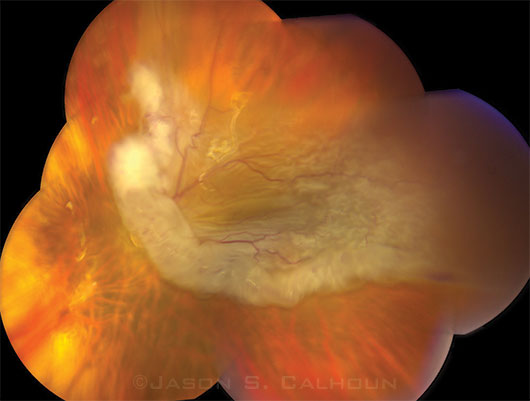 |
Myopia Complication. Retinal detachment is among the many potential complications of high myopia.
|
Urbanization. “Several groups, including ours, have shown that urban populations have a higher risk of myopia,” said Prof. Tan. But longer hours of study and near work combined with fewer outdoor activities likely also come into play, he said.
In rural, low-resource areas where there is less access to education or development, the level of myopia is often low—somewhere between 2% and 5%, said Dr. Flitcroft. “Left to its own devices and without the influences of modernization, the system that controls refractive development seems to work very well.”
Wealth. “We often talk about the myopia differences between urban and rural populations,” said Prof. Congdon. “But it’s more likely an issue of rich versus poor.” Earlier this year, Prof. Congdon published an article in Ophthalmology, examining 2 adjoining populations—1 middle-income, 1 low-income. There was a big difference in myopia—with the wealthier cohort at greater risk—but not a big difference in time spent outdoors or with near work.8
Researchers have explored other potential links to standard of living such as improved diet, which can mean that kids grow taller, he said. But increased height hasn’t appeared to coexist with bigger, more myopic eyes. “We also looked at stunting as a measure of nutrition and found no inverse association with myopia,” said Prof. Congdon.
“There is a large amount of evidence that behavioral factors such as outdoor activity and near work are important,” he said, “but based on our studies, I’m not convinced they fully explain the growing prevalence we’re seeing. There may be other factors associated with wealth and development that we don’t yet fully understand.”
 |
Research. Dr. Congdon measures axial length using ultrasound, as his group is studying factors that influence myopia in kids.
|
Primary Prevention
A 2011 Cochrane review has provided evidence that optical interventions and pharmacology can help slow rates of myopia.9
Pharmaceutical approach: atropine. Thus far, muscarinic receptor antagonists, especially atropine eyedrops, have demonstrated the largest effect in slowing axial elongation and myopic progression.9
Efficacy. Prof. Tan has completed 2 major randomized atropine trials, the first in 1999. “Our studies concentrated on children between the ages of 6 and 12, when myopia tends to progress,” said Prof. Tan. He and his colleagues have tested 4 different doses—0.01, 0.1, 0.5, and 1%. With the highest dose, they were able to slow progression by about 78%. “But we were also able to retard progression with a very low dose (0.01%) by about 50% to 60%,” he said. In a subset of patients, however, progression is more aggressive—even with treatment. “For these patients, 0.01% may not be adequate, and we may need to increase the dosage,” said Prof. Tan.
Side effects. Not a big proponent of atropine, Dr. Young remains concerned about daily absorption through the nasolacrimal system. However, Prof. Tan said that systemic effects appear to be minimal. The highest dose does cause greater ocular side effects, though, such as light sensitivity and blurry near vision, he said. It also leads to greater rebound (increased progression and eye growth) after treatment is stopped.10
On the other hand, the very low dose produces minimal ocular side effects, said Prof. Tan, including pupil dilation of about 1 mm or less and without significant impairment of near vision.11 The lowest dose offers another advantage—fewer allergic reactions.
Mechanism of action. “Although we don’t really understand how atropine works,” said Prof. Tan, “we do believe that it is not by blocking accommodation, a theory that was disproven with animal models.” Other theories suggest that atropine may slow eye growth by working either on muscarinic receptors in the retina or directly on scleral fibroblasts by non-muscarinic receptors.
More research needed. To date, atropine studies have been primarily conducted in East and Southeast Asia, said Dr. Flitcroft. In the United States, 1% atropine is FDA approved for penalization therapy in children with amblyopia. “But atropine is not widely accepted [for myopia] in the West,” said Dr. Flitcroft, who is currently applying for research funds to conduct an atropine-myopia trial in Europe and obtain more evidence. It would also be helpful to get good follow-up data from Taiwan, said Prof. Morgan, where high doses of atropine have been used in large numbers of children for about 20 years.
A similar agent. Phase 1 and 2 trials in the United States and in East and Southeast Asia found another muscarinic antagonist agent—pirenzepine (2% gel)—less effective than atropine, and with more surface allergy issues; however, it causes less cycloplegia and mydriasis, said Dr. Flitcroft. “Although pirenzepine is no longer under development for commercial reasons, its treatment effect was similar in both populations.”
Optical approaches. In a few small studies, optical approaches show statistically significant treatment benefits, said Prof. Tan, and contact lenses appear more promising than spectacles.
Peripheral defocus contact lenses. One new optical treatment is based on the theory that axial eye growth is influenced by blurred vision in the peripheral retina, said Prof. Tan. “Hyperopic blur will accelerate axial growth,” said Dr. Flitcroft, “but inducing myopic blur in the periphery will tend to slow it down. With these new lenses, it is possible to slow axial growth by 30% to 50%.” Similar to traditional bifocals or multifocals, said Dr. Young, the center part of the multifocal lenses corrects nearsightedness, while progressive rings correct peripheral hyperopia. “I prescribe them for older children,” she said, “but ideally, you would use them in patients as young as 4 with early myopia and a family history of the condition.” However, they are hard to sustain as a treatment option in patients at this age, she said, because it can be difficult to get consistent cooperation from these young children.
Orthokeratology (Ortho-K). Although Ortho-K has long been used as a temporary treatment for existing myopia in adults, it is now being studied as a way to slow progression of myopia in children. These rigid contact lenses are worn while the patient is asleep to remodel the corneal shape, said Dr. Flitcroft. They create an effect that is optically similar to peripheral defocus contact lenses, he said, by shaping the cornea so as to change the off-axis defocus on the retina in the direction that slows down axial growth, reducing hyperopic blur in the periphery.
Several randomized trials are beginning to show that long-term use of Ortho-K may reduce marked progression by as much as 43%, said Prof. Tan.12 “With long-term lens wear, however, comes a high risk of infection. Although these are rigid gas permeable lenses,” he added, “the odds ratio of risk with Ortho-K use in children is as high as the risk of adults wearing soft contact lenses overnight.” There are at least 150 cases of infection reported in the literature, he said, including very severe ones caused by Pseudomonas and Acanthamoeba.
In addition to infection and compliance issues from discomfort, said Dr. Young, the cornea resumes its previous shape in about a week after the lens is removed, so long-term results may be less encouraging. However, said Dr. Flitcroft, recent studies show that Ortho-K is affecting eye growth and having an impact on axial length.
___________________________
1 Ma X et al. Br Med J. 2014;349:g5740.
2 Flitcroft I. Prog Retin Eye Res. 2012;31(6):622-660.
3 Flitcroft I. Eye. 2014;28(2):169-179.
4 Sherwin JC et al. Ophthalmology. 2012;119(10):2141-2151.
5 Ciuffreda KJ et al. Vision Res. 2007;47(9):1245-1252.
6 McKnight CM et al. Am J Ophthalmol. 2014;158(5):1079-1085.
7 Williams K et al. Ophthalmology. 2015;122(7):1489-1497.
8 Zhongqiang Z et al. Ophthalmology. 2015;122(5):1060-1062.
9 Walline JJ et al. Cochrane Database Syst Rev. 2011;12:CD004916.
10 Chia A et al. Am J Ophthalmol. 2014;157(2):451-457.
11 Chia A et al. Ophthalmology. Aug. 11, 2015 [Epub ahead of print].
12 Sun Y et al. PLoS One. 2015;10(4):e0124535.
Meet the Experts
Nathan G. Congdon, MD, MPH Professor, State Key Laboratory of Ophthalmology and Division of Preventive Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, China; and professor, Queen’s University Belfast, Northern Ireland. Relevant financial disclosures: Essilor: S.
Ian Flitcroft, DPhil, FRCOphth Ophthalmologist, Children’s University Hospital, Dublin, Ireland. Relevant financial disclosures: None.
Ian G. Morgan, PhD Scientist, Research School of Biology, Australian National University, Canberra, Australia; Division of Preventive Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, China. Relevant financial disclosures: Novartis Japan: L.
Donald Tan, MD, FRCS, FRCOphth Arthur Lim Professor, Ophthalmology and Visual Sciences Academic Clinical Program, Duke-National University of Singapore Graduate Medical School, senior consultant, Singapore National Eye Centre. Relevant financial disclosures: None.
Katie M. Williams, MPhil, FRCOphth MRC clinical research fellow, Department of Ophthalmology, King’s College London, St. Thomas’ Hospital, London, United Kingdom; Department of Twin Research and Genetic Epidemiology, King’s College London, St. Thomas’ Hospital, London, United Kingdom. Relevant financial disclosures: None.
Terri L. Young, MD, MBA Pediatric ophthalmologist and geneticist; professor and chair of Ophthalmology and Visual Sciences, University of Wisconsin School of Medicine and Public Health, Madison, Wisc. Relevant financial disclosures: None.
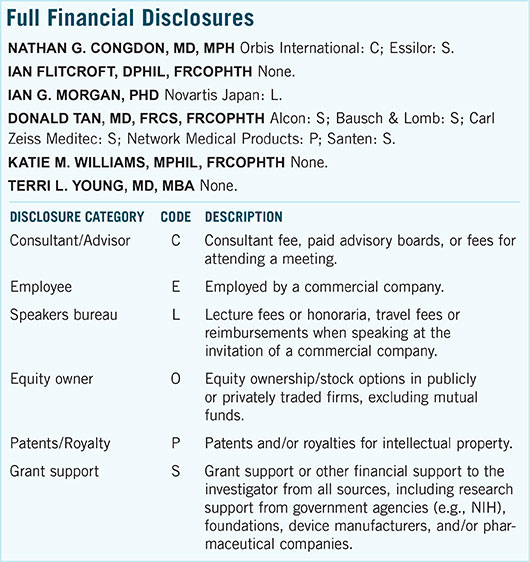
For full disclosures and the disclosure key, see below.
|